Abstract
Research Article
Enhancing adipose stem cell chondrogenesis: A study on the roles of dexamethasone, transforming growth factor β3 and ascorbate supplements and their combination
Bernard J Van Wie*, Arshan Nazempour##, Chrystal R Quisenberry## and Nehal I Abu-Lail
Published: 31 July, 2017 | Volume 1 - Issue 1 | Pages: 028-051
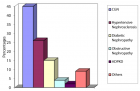
Varied exogenous chondrogenic factors (CFs) are implicated in promoting differentiation of stem cells along a chondrocyte lineage in the field of regenerative tissue engineering for articular cartilage repair. The effects of dexamethasone, transforming growth factor β3 (TGF-β3), ascorbate, and their combinations, on mRNA expression in micromass-cultured human adipose derived stem cells (hADSCs) were investigated as a function of time. Indices include chondrogenic, hypertrophic, angiogenic, fibrogenic and osteogenic markers along with mechanical properties, assessed by atomic force microscopy. Early in the culture, i.e., at day three, no significant differences in mRNA expression of SOX9, aggrecan, lubricin, Col XI, Col X, vascular endothelial growth factor, Col I, and alkaline phosphatase were observed among samples treated with different CFs. However, significant differences in mRNA expression levels of pre-mentioned markers among samples treated with each CF exist when samples were supplied with the CFs for more than three days. A new indexing scheme summing expression of chondrogenic and subtracting non-chondrogenic angiogenic, fibrogenic and osteogenic marker levels shows dexamethasone is the overall leading CF among the factors and their combinations. Based on this scheme, we have projected not only the possible signaling pathways which might be affected by addition of CFs but also hypothetical indexes that may occur upon temporal variation of growth factor regimens.
Read Full Article HTML DOI: 10.29328/journal.jsctt.1001004 Cite this Article Read Full Article PDF
Keywords:
Ascorbate; Atomic force microscopy; Elastic modulus; Cartilage; Chondrogenesis; Dexamethasone; Transforming growth factor β3 and Human-adipose derived stem cells
References
- Longo UG, Petrillo S, Franceschetti E, Berton A, Maffulli N, et al. Stem Cells and Gene Therapy for Cartilage Repair. Stem Cells Int. 2012; 2012: 168385. Ref.: https://goo.gl/B8pCeK
- Buckwalter JA. Articular cartilage: injuries and potential for healing. J Orthop Sports Phys Ther. 1998; 28: 192-202. Ref.: https://goo.gl/QYV1E8
- Lee CR, Grodzinsky AJ, Hsu HP, Martin SD, Spector M. Effects of harvest and selected cartilage repair procedures on the physical and biochemical properties of articular cartilage in the canine knee. J Orthop Res. 2000; 18: 790-799. Ref.: https://goo.gl/poz8Kr
- Darling EM, Athanasiou KA. Rapid phenotypic changes in passaged articular chondrocyte subpopulations. J Orthop Res. 2005; 23: 425-432. Ref.: https://goo.gl/bztYZU
- Winter A, Breit S, Parsch D, Benz K, Steck E, et al. Cartilage-like gene expression in differentiated human stem cell spheroids: A comparison of bone marrow-derived and adipose tissue-derived stromal cells. Arthritis Rheum. 2003; 48: 418-429. Ref.: https://goo.gl/XMpcXN
- Grigolo B, Lisignoli G, Desando G, Cavallo C, Marconi E, et al. Osteoarthritis treated with mesenchymal stem cells on hyaluronan-based scaffold in rabbit. Tissue Eng Part C Methods. 2009; 15: 647-658. Ref.: https://goo.gl/CTeKm8
- Al Faqeh H, Nor Hamdan BM, Chen HC, Aminuddin BS, Ruszymah BH. The potential of intra-articular injection of chondrogenic-induced bone marrow stem cells to retard the progression of osteoarthritis in a sheep model. Exp Gerontol. 2012; 47: 458-464. Ref.: https://goo.gl/WDGPnX
- Murphy JM, Fink DJ, Hunziker EB, Barry FP. Stem cell therapy in a caprine model of osteoarthritis. Arthritis Rheum. 2003; 48: 3464-3474. Ref.: https://goo.gl/6CnJo9
- Sato M, Uchida K, Nakajima H, Miyazaki T, Guerrero AR, et al. Direct transplantation of mesenchymal stem cells into the knee joints of Hartley strain guinea pigs with spontaneous osteoarthritis. Arthritis Res Ther. 2012; 14: 31. Ref.: https://goo.gl/mUC9vs
- Wakitani S, Nawata M, Tensho K, Okabe T, Machida H, et al. Repair of articular cartilage defects in the patello-femoral joint with autologous bone marrow mesenchymal cell transplantation: three case reports involving nine defects in five knees. J Tissue Eng Regen Med. 2007; 1: 74-79. Ref.: https://goo.gl/YYmTif
- Lee RH, Kim B, Choi I, Kim H. Characterization and expression analysis of mesenchymal stem cells from human bone marrow and adipose tissue. Cell Physiol Biochem. 2004; 14: 311-324. Ref.: https://goo.gl/pJY7WG
- Ogawa R, Mizuno S, Murphy GF, Orgill DP. The effect of hydrostatic pressure on three-dimensional chondroinduction of human adipose-derived stem cells. Tissue Eng Part A. 2009; 15: 2937-2945. Ref.: https://goo.gl/vu6nK1
- Gimble J, Guilak F. Adipose-derived adult stem cells: isolation, characterization, and differentiation potential. Cytotherapy. 2003; 5: 362-369. Ref.: https://goo.gl/oCTsHr
- Schmid TM, Linsenmayer TF. Immunohistochemical localization of short chain cartilage collagen (type X) in avian tissues. J Cell Biol. 1985; 100: 598-605. Ref.: https://goo.gl/6WtKcS
- Wegger I, Palludan B. Vitamin C deficiency causes hematological and skeletal abnormalities during fetal development in swine. J Nutr. 1994; 124: 241-248. Ref.: https://goo.gl/Q92ZLn
- van der Kraan PM, Davidson ENB, Blom A, van den Berg WB. TGF-beta signaling in chondrocyte terminal differentiation and osteoarthritis Modulation and integration of signaling pathways through receptor-Smads. Osteoarthritis Cartilage 2009; 17: 1539-1545. Ref.: https://goo.gl/yY2PDQ
- Walsh S, Jordan GR, Jefferiss C, Stewart K, Beresford JN. High concentrations of dexamethasone suppress the proliferation but not the differentiation or further maturation of human osteoblast precursors in vitro: relevance to glucocorticoid-induced osteoporosis. Rheumatology. 2001; 40: 74-83. Ref.: https://goo.gl/nhwSE6
- Hong L, Sultana H, Paulius K, Zhang G. Steroid regulation of proliferation and osteogenic differentiation of bone marrow stromal cells: a gender difference. J Steroid Biochem Mol Biol. 2009; 114: 180-185. Ref.: https://goo.gl/kiKjkH
- Derfoul A, Perkins GL, Hall DJ, Tuan RS. Glucocorticoids promote chondrogenic differentiation of adult human mesenchymal stem cells by enhancing expression of cartilage extracellular matrix genes. Stem Cells. 2006; 24: 1487-1495. Ref.: https://goo.gl/utBa5T
- Nazempour A, Wie BJ. Chondrocytes, Mesenchymal Stem Cells, and Their Combination in Articular Cartilage Regenerative Medicine. Ann Biomed Eng. 2016; 1325-1354. Ref.: https://goo.gl/tKMNpd
- Cals FL, Hellingman CA, Koevoet W, Baatenburg de Jong RJ, van Osch GJ. Effects of transforming growth factor-beta subtypes on in vitro cartilage production and mineralization of human bone marrow stromal-derived mesenchymal stem cells. J Tissue Eng Regen Med. 2012; 6: 68-76. Ref.: https://goo.gl/6Xqi3z
- Awad HA, Halvorsen YD, Gimble JM, Guilak F. Effects of transforming growth factor beta1 and dexamethasone on the growth and chondrogenic differentiation of adipose-derived stromal cells. Tissue Eng. 2003; 9: 1301-1312. Ref.: https://goo.gl/eXiXWo
- Altaf FM, Hering TM, Kazmi NH, Yoo JU, Johnstone B. Ascorbate-enhanced chondrogenesis of ATDC5 cells. Eur Cell Mater. 2006; 12: 64-70. Ref.: https://goo.gl/HzZ6tp
- Xu Y, Balooch G, Chiou M, Bekerman E, Ritchie RO, et al. Analysis of the material properties of early chondrogenic differentiated adipose-derived stromal cells (ASC) using an in vitro three-dimensional micromass culture system. Biochem Biophys Res Commun. 2007; 359: 311-316. Ref.: https://goo.gl/PAFcRF
- Stott NS, Jiang TX, Chuong CM. Successive formative stages of precartilaginous mesenchymal condensations in vitro: modulation of cell adhesion by Wnt-7A and BMP-2. J Cell Physiol. 1999; 180: 314-324. Ref.: https://goo.gl/mpFKzn
- Ahrens PB, Solursh M, Reiter RS. Stage-related capacity for limb chondrogenesis in cell culture. Dev Biol. 1977; 60: 69-82. Ref.: https://goo.gl/HScfBL
- Carlberg AL, Pucci B, Rallapalli R, Tuan RS, Hall DJ. Efficient chondrogenic differentiation of mesenchymal cells in micromass culture by retroviral gene transfer of BMP-2. Differentiation. 2001; 67: 128-138. Ref.: https://goo.gl/njGqNs
- Hou C, Zhang Z, Zhang Z, Wu P, Zhao X, et al. Presence and function of microRNA-92a in chondrogenic ATDC5 and adipose-derived mesenchymal stem cells. Mol Med Rep. 2015; 12: 4877-4886. Ref.: https://goo.gl/WV8bEL
- Yang JW, de Isla N, Huselstein C, Sarda-Kolopp MN, Li N, et al. Evaluation of human MSCs cell cycle, viability and differentiation in micromass culture. Biorheology. 2006; 43: 489-496. Ref.: https://goo.gl/JM39oi
- Zhang L, Su P, Xu C, Yang J, Yu W, et al. Chondrogenic differentiation of human mesenchymal stem cells: a comparison between micromass and pellet culture systems. Biotechnol Lett. 2010; 32: 1339-1346. Ref.: https://goo.gl/iqgdYb
- Johnston S, Siegel C. Comparison of a serum replacement (Omni Serum) and fetal bovine serum in cell cultures used to isolate herpes simplex virus from clinical specimens. J Clin Microbiol. 1990; 28: 643-645. Ref.: https://goo.gl/QrW1V5
- Vavken P, Arrich F, Pilz M, Dorotka R. An in vitro model of biomaterial-augmented microfracture including chondrocyte-progenitor cell interaction. Arch Orthop Trauma Surg. 2010; 130: 711-716. Ref.: https://goo.gl/zJDW5m
- Ryu JS, Jung YH, Cho MY, Yeo JE, Choi YJ, et al. Co-culture with human synovium-derived mesenchymal stem cells inhibits inflammatory activity and increases cell proliferation of sodium nitroprusside-stimulated chondrocytes. Biochem Biophys Res Commun. 2014; 447: 715-720. Ref.: https://goo.gl/3g751G
- Xu L, Wang Q, Xu F, Ye Z, Zhou Y, et al. Mesenchymal stem cells downregulate articular chondrocyte differentiation in noncontact coculture systems: implications in cartilage tissue regeneration. Stem Cells Dev. 2013; 22: 1657-1669. Ref.: https://goo.gl/bKYdTD
- Lai JH, Kajiyama G, Smith RL, Maloney W, Yang F. Stem cells catalyze cartilage formation by neonatal articular chondrocytes in 3D biomimetic hydrogels. Sci Rep. 2013; 3: 3553. Ref.: https://goo.gl/N4XY4D
- Lopa S, Colombini A, Sansone V, Preis FW, Moretti M. Influence on chondrogenesis of human osteoarthritic chondrocytes in co-culture with donor-matched mesenchymal stem cells from infrapatellar fat pad and subcutaneous adipose tissue. Int J Immunopathol Pharmacol. 2013; 26: 23-31. Ref.: https://goo.gl/BR8cs9
- Leyh M, Seitz A, Dürselen L, Schaumburger J, Ignatius A, et al. Subchondral bone influences chondrogenic differentiation and collagen production of human bone marrow-derived mesenchymal stem cells and articular chondrocytes. Arthritis Res Ther. 2014; 16: 453. Ref.: https://goo.gl/Fmy7TC
- Schmittgen TD, Livak KJ. Analyzing real-time PCR data by the comparative C(T) method. Nat Protoc. 2008; 3: 1101-1108. Ref.: https://goo.gl/7K2R5h
- Harada M, Mitsuyama K, Yoshida H, Sakisaka S, Taniguchi E, et al. Vascular endothelial growth factor in patients with rheumatoid arthritis. Scand J Rheumatol. 1998; 27: 377-380. Ref.: https://goo.gl/RHxUFZ
- Abu-Lail NI, Camesano TA. The effect of solvent polarity on the molecular surface properties and adhesion of Escherichia coli. Colloids Surf B Biointerfaces. 2006; 51: 62-70. Ref.: https://goo.gl/KeDLSz
- Barquins M, Maugis D. Adhesive contact of axisymmetric punches on an elastic half-space-the modified Hertz-Hubers stress tensor for contacting spheres. Journal de Mecanique theorique et appliquee. 1982; 1: 331-357.
- Park B-J, Abu-Lail NI. Variations in the Nanomechanical Properties of Virulent and Avirulent Listeria monocytogenes. Soft matter. 2010; 6: 3898-3909. Ref.: https://goo.gl/eCJoX8
- Long R, Hall Matthew S, Wu M, Hui CY. Effects of Gel Thickness on Microscopic Indentation Measurements of Gel Modulus. Biophysical Journal. 2011; 101: 643-650. Ref.: https://goo.gl/PhzTet
- Santos J, Rebêlo L, Araujo A, Barrosa EB, de Sousa JS. Thickness-corrected model for nanoindentation of thin films with conical indenters. Soft Matter. 2012; 8: 4441-4448. Ref.: https://goo.gl/tNJVJN
- Fischer-Cripps AC. The Hertzian contact surface. Journal of Materials Science. 1999; 34: 129-137. Ref.: https://goo.gl/MRyHZt
- Nazempour A, Quisenberry CR, Van Wie BJ, Abu-Lail NI. Nanomechanics of engineered articular cartilage: synergistic influences of transforming growth factor-β3 and oscillating pressure. J Nanosci Nanotechnol. 2016; 16: 3136-3145. Ref.: https://goo.gl/tKpzxd
- Yuan JS, Reed A, Chen F, Stewart CN Jr. Statistical analysis of real-time PCR data. BMC Bioinformatics. 2006; 7: 85. Ref.: https://goo.gl/mJ47oj
- Kern JA, Lamb RJ, Reed JC, Daniele RP, Nowell PC. Dexamethasone inhibition of interleukin 1 beta production by human monocytes. Posttranscriptional mechanisms. J Clin Invest. 1998; 81: 237-244. Ref.: https://goo.gl/Ph3eKD
- Stewart AA, Byron CR, Pondenis HC, Stewart MC. Effect of dexamethasone supplementation on chondrogenesis of equine mesenchymal stem cells. Am J Vet Res. 2008; 69: 1013-1021. Ref.: https://goo.gl/Ltk1H1
- Hall BK. Chapter 23-Cartilage Diversity. Bones and Cartilage (Second Edition). San Diego: Academic Press. 2015; 387-400.
- Acharya C, Adesida A, Zajac P, Mumme M, Riesle J, et al. Enhanced chondrocyte proliferation and mesenchymal stromal cells chondrogenesis in coculture pellets mediate improved cartilage formation. J Cell Physiol. 2012; 227: 88-97. Ref.: https://goo.gl/XWE97D
- Bruce SJ, Butterfield NC, Metzis V, Town L, McGlinn E, et al. Inactivation of Patched1 in the mouse limb has novel inhibitory effects on the chondrogenic program. J Biol Chem. 2010; 285: 27967-27981. Ref.: https://goo.gl/9KRgv9
- Kalwitz G, Neumann K, Ringe J, Sezer O, Sittinger M, et al. Chondrogenic differentiation of human mesenchymal stem cells in micro-masses is impaired by high doses of the chemokine CXCL7. Journal of Tissue Engineering and Regenerative Medicine. 2011; 5: 50-59. Ref.: https://goo.gl/R1ox1N
- Cooke ME, Allon AA, Cheng T, Kuo AC, Kim HT, et al. Structured three-dimensional co-culture of mesenchymal stem cells with chondrocytes promotes chondrogenic differentiation without hypertrophy. Osteoarthritis Cartilage. 2011; 19: 1210-1218. Ref.: https://goo.gl/Ehp8qj
- Tanaka H, Murphy CL, Murphy C, Kimura M, Kawai S, et al. Chondrogenic differentiation of murine embryonic stem cells: effects of culture conditions and dexamethasone. J Cell Biochem. 2004; 93: 454-462. Ref.: https://goo.gl/3FK6sP
- Zhou H, Mak W, Kalak R, Street J, Fong-Yee C, et al. Glucocorticoid-dependent Wnt signaling by mature osteoblasts is a key regulator of cranial skeletal development in mice. Development. 2009; 136: 427-436. Ref.: https://goo.gl/8Xw9Ty
- Lee MJ, Fried SK. The glucocorticoid receptor, not the mineralocorticoid receptor, plays the dominant role in adipogenesis and adipokine production in human adipocytes. Int J Obes (Lond). 2014; 38: 1228-1233. Ref.: https://goo.gl/gTL21q
- Huang JI, Zuk PA, Jones NF, Zhu M, Lorenz HP, et al. Chondrogenic potential of multipotential cells from human adipose tissue. Plast Reconstr Surg. 2004; 113: 585-594. Ref.: https://goo.gl/q6ZTy4
- Kim HJ, Im GI. Chondrogenic differentiation of adipose tissue-derived mesenchymal stem cells: greater doses of growth factor are necessary. J Orthop Res. 2009; 27: 612-619. Ref.: https://goo.gl/2grnMs
- Akiyama H. Control of chondrogenesis by the transcription factor Sox9. Mod Rheumatol. 2008; 18: 213-219. Ref.: https://goo.gl/1Zidcn
- Diao HJ, Yeung CW, Yan CH, Chan GC, Chan BP. Bidirectional and mutually beneficial interactions between human mesenchymal stem cells and osteoarthritic chondrocytes in micromass co-cultures. Regen Med. 2013; 8: 257-269. Ref.: https://goo.gl/x3ryDx
- von der Mark K, Gauss V, von der Mark H, Müller P. Relationship between cell shape and type of collagen synthesised as chondrocytes lose their cartilage phenotype in culture. Nature. 1977; 267: 531-532. Ref.: https://goo.gl/dgXyQ1
- Hao H, Chen G, Liu J, Ti D, Zhao Y, et al. Culturing on Wharton's jelly extract delays mesenchymal stem cell senescence through p53 and p16INK4a/pRb pathways. Plos One. 2013; 8: 13. Ref.: https://goo.gl/1VQYzp
- Kawakami Y, Rodriguez-Leon J, Izpisua Belmonte JC. The role of TGFbetas and Sox9 during limb chondrogenesis. Curr Opin Cell Biol. 2006; 18: 723-729. Ref.: https://goo.gl/KeXmDG
- Bell DM, Leung KK, Wheatley SC, Ng LJ, Zhou S, et al. SOX9 directly regulates the type-II collagen gene. Nat Genet. 1997; 16: 174-178. Ref.: https://goo.gl/Wg7v9R
- Rich JT, Rosova I, Nolta JA, Myckatyn TM, Sandell LJ, et al. Upregulation of Runx2 and Osterix during in vitro chondrogenesis of human adipose-derived stromal cells. Biochem Biophys Res Commun. 2008; 372: 230-235. Ref.: https://goo.gl/r6rpbM
- Shintani N, Hunziker EB. Differential effects of dexamethasone on the chondrogenesis of mesenchymal stromal cells: influence of microenvironment, tissue origin and growth factor. Eur Cell Mater. 2011; 22: 302-319. Ref.: https://goo.gl/gM4uyi
- Diekman BO, Rowland CR, Lennon DP, Caplan AI, Guilak F. Chondrogenesis of Adult Stem Cells from Adipose Tissue and Bone Marrow: Induction by Growth Factors and Cartilage-Derived Matrix. Tissue Engineering Part A. 2010; 16: 523-533. Ref.: https://goo.gl/V7vvwk
- Aung A, Gupta G, Majid G, Varghese S. Osteoarthritic chondrocyte-secreted morphogens induce chondrogenic differentiation of human mesenchymal stem cells. Arthritis Rheum. 2011; 63: 148-158. Ref.: https://goo.gl/8QsMKd
- Jay GD, Waller KA. The biology of lubricin: near frictionless joint motion. Matrix Biol. 2014; 39: 17-24. Ref.: https://goo.gl/RHZHnD
- Waller KA, Zhang LX, Elsaid KA, Fleming BC, Warman ML, et al. Role of lubricin and boundary lubrication in the prevention of chondrocyte apoptosis. Proceedings of the National Academy of Sciences. 2013; 110: 5852-5857. Ref.: https://goo.gl/Va5tbac
- Jones AR, Flannery CR. Bioregulation of lubricin expression by growth factors and cytokines. Eur Cell Mater. 2007; 13: 40-45. Ref.: https://goo.gl/nE4N29
- Eyre D. Articular cartilage and changes in Arthritis: Collagen of articular cartilage. Arthritis Research & Therapy. 2001; 4: 1-6. Ref.: https://goo.gl/k7dQCf
- Sophia Fox AJ, Bedi A, Rodeo SA. The Basic Science of Articular Cartilage: Structure, Composition, and Function. Sports Health. 2009; 1: 461-468. Ref.: https://goo.gl/dL8txZ
- Spranger J. The type XI collagenopathies. Pediatr Radiol. 1998; 28: 745-750. Ref.: https://goo.gl/J45AZN
- Kwan AP, Cummings CE, Chapman JA, Grant ME. Macromolecular organization of chicken type X collagen in vitro. J Cell Biol. 1991; 114: 597-604. Ref.: https://goo.gl/zgy2wx
- Mwale F, Stachura D, Roughley P, Antoniou J. Limitations of using aggrecan and type X collagen as markers of chondrogenesis in mesenchymal stem cell differentiation. J Orthop Res. 2006; 24: 1791-1798. Ref.: https://goo.gl/i3jy5n
- Bengoetxea H, Argandoña EG, Lafuente Jé V. Effects of Visual Experience on Vascular Endothelial Growth Factor Expression during the Postnatal Development of the Rat Visual Cortex. Cereb Cortex. 2008; 18: 1630-1639. Ref.: https://goo.gl/HyoGKP
- Giatromanolaki A, Sivridis E, Athanassou N, Zois E, Thorpe PE, et al. The angiogenic pathway ‘vascular endothelial growth factor/flk-1(KDR)-receptor’ in rheumatoid arthritis and osteoarthritis. The Journal of Pathology. 2001; 194: 101-108. Ref.: https://goo.gl/CJLPpt
- Rehman J, Traktuev D, Li J, Merfeld-Clauss S, Temm-Grove CJ, et al. Secretion of angiogenic and antiapoptotic factors by human adipose stromal cells. Circulation. 2004; 109: 1292-1298. Ref.: https://goo.gl/1NioEG
- Lee CS, Watkins E, Burnsed OA, Schwartz Z, Boyan BD. Tailoring adipose stem cell trophic factor production with differentiation medium components to regenerate chondral defects. Tissue Eng Part A. 2013; 19: 1451-1464. Ref.: https://goo.gl/t1cELW
- Sandell LJ, Aigner T. Articular cartilage and changes in arthritis. An introduction: cell biology of osteoarthritis. Arthritis Res. 2001; 3: 107-113. Ref.: https://goo.gl/rfBqgB
- Diekman BO, Estes BT, Guilak F. The effects of BMP6 overexpression on adipose stem cell chondrogenesis: Interactions with dexamethasone and exogenous growth factors. J Biomed Mater Res A. 2010; 93: 994-1003. Ref.: https://goo.gl/k9ujzV
- Tapp H, Deepe R, Ingram JA, Kuremsky M, Hanley EN Jr, et al. Adipose-derived mesenchymal stem cells from the sand rat: transforming growth factor beta and 3D co-culture with human disc cells stimulate proteoglycan and collagen type I rich extracellular matrix. Arthritis Res Ther. 2008; 10: 89. Ref.: https://goo.gl/cc9aPq
- Birmingham E, Niebur GL, McHugh PE, Shaw G, Barry FP, et al. Osteogenic differentiation of mesenchymal stem cells is regulated by osteocyte and osteoblast cells in a simplified bone niche. Eur Cell Mater. 2012; 23: 13-27. Ref.: https://goo.gl/iTasgi
- Miao D, Scutt A. Histochemical localization of alkaline phosphatase activity in decalcified bone and cartilage. J Histochem Cytochem. 2002; 50: 333-340. Ref.: https://goo.gl/9hZLFH
- Cimmino MA, Buffrini L, Barisone G, Bruzzone M, Accardo S. Alkaline phosphatase activity in the serum of patients with rheumatoid arthritis. Z Rheumatol. 1990; 49: 143-146. Ref.: https://goo.gl/EPFDBA
- Langenbach F, Handschel J. Effects of dexamethasone, ascorbic acid and β-glycerophosphate on the osteogenic differentiation of stem cells in vitro. Stem Cell Research & Therapy. 2013; 4: 117-117. Ref.: https://goo.gl/7avFxi
- Westhrin M, Xie M, Olderoy MO, Sikorski P, Strand BL, et al. Osteogenic differentiation of human mesenchymal stem cells in mineralized alginate matrices. PLoS One. 2015; 10: 0120374. Ref.: https://goo.gl/KGcCQG
- Cruz AC, Silva ML, Caon T, Simões CM. Addition of bone morphogenetic protein type 2 to ascorbate and beta-glycerophosphate supplementation did not enhance osteogenic differentiation of human adipose-derived stem cells. J Appl Oral Sci. 2012; 20: 628-635. Ref.: https://goo.gl/u1itzK
- Nakashima K, Zhou X, Kunkel G, Zhang Z, Deng JM, et al. The novel zinc finger-containing transcription factor osterix is required for osteoblast differentiation and bone formation. Cell. 2002; 108: 17-29. Ref.: https://goo.gl/YMfdA2
- Zhu F, Friedman MS, Luo W, Woolf P, Hankenson KD. The transcription factor osterix (SP7) regulates BMP6-induced human osteoblast differentiation. J Cell Physiol. 2012; 227: 2677-2685. Ref.: https://goo.gl/tW4sYJ
- Nishimura R, Wakabayashi M, Hata K, Matsubara T, Honma S, et al. Osterix regulates calcification and degradation of chondrogenic matrices through matrix metalloproteinase 13 (MMP13) expression in association with transcription factor Runx2 during endochondral ossification. J Biol Chem. 2012; 287: 33179-33190. Ref.: https://goo.gl/Pwe3xi
- Aguiari P, Leo S, Zavan B, Vindigni V, Rimessi A, et al. High glucose induces adipogenic differentiation of muscle-derived stem cells. Proc Natl Acad Sci U S A. 2008; 105: 1226-1231. Ref.: https://goo.gl/PwnAk8
- Chuang CC, Yang RS, Tsai KS, Ho FM, Liu SH. Hyperglycemia enhances adipogenic induction of lipid accumulation: involvement of extracellular signal-regulated protein kinase 1/2, phosphoinositide 3-kinase/Akt, and peroxisome proliferator-activated receptor gamma signaling. Endocrinology. 2007; 148: 4267-4275. Ref.: https://goo.gl/TMWZnD
- Tsai TL, Manner PA, Li WJ. Regulation of mesenchymal stem cell chondrogenesis by glucose through protein kinase C/transforming growth factor signaling. Osteoarthritis Cartilage. 2013; 21: 368-376. Ref.: https://goo.gl/RsN5u9
- Advani S, LaFrancis D, Bogdanovic E, Taxel P, Raisz LG, et al. Dexamethasone suppresses in vivo levels of bone collagen synthesis in neonatal mice. Bone. 1997; 20: 41-46. Ref.: https://goo.gl/yz3ij7
- Mackay AM, Beck SC, Murphy JM, Barry FP, Chichester CO, et al. Chondrogenic differentiation of cultured human mesenchymal stem cells from marrow. Tissue Engineering. 1998; 4: 415-428. Ref.: https://goo.gl/FZFNR1
- Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, et al. Multilineage potential of adult human mesenchymal stem cells. Science. 1999; 284: 143-147. Ref.: https://goo.gl/xQKrQG
- Towle CA, Hung HH, Bonassar LJ, Treadwell BV, Mangham DC. Detection of interleukin-1 in the cartilage of patients with osteoarthritis: a possible autocrine/paracrine role in pathogenesis. Osteoarthritis and Cartilage. 1997; 5: 293-300. Ref.: https://goo.gl/FraFzS
- Huh JE, Koh PS, Seo BK, Park YC, Baek YH, et al. Mangiferin reduces the inhibition of chondrogenic differentiation by IL-1beta in mesenchymal stem cells from subchondral bone and targets multiple aspects of the Smad and SOX9 pathways. Int J Mol Sci. 2014; 15: 16025-16042. Ref.: https://goo.gl/bG1sBe
- Kunz D, Walker G, Eberhardt W, Pfeilschifter J. Molecular mechanisms of dexamethasone inhibition of nitric oxide synthase expression in interleukin 1 beta-stimulated mesangial cells: evidence for the involvement of transcriptional and posttranscriptional regulation. Proceedings of the National Academy of Sciences. 1996; 93: 255-259. Ref.: https://goo.gl/xr1qbL
- Tangtrongsup S, Kisiday JD. Effects of Dexamethasone Concentration and Timing of Exposure on Chondrogenesis of Equine Bone Marrow-Derived Mesenchymal Stem Cells. Cartilage. 2016; 7: 92-103. Ref.: https://goo.gl/ScQCAh
- Lee SW, Tsou AP, Chan H, Thomas J, Petrie K, et al. Glucocorticoids selectively inhibit the transcription of the interleukin 1 beta gene and decrease the stability of interleukin 1 beta mRNA. Proc Natl Acad Sci U S A. 1988; 85: 1204-1208. Ref.: https://goo.gl/q4FRna
- Leonard CM, Fuld HM, Frenz DA, Downie SA, Massagué J, et al. Role of transforming growth factor-beta in chondrogenic pattern formation in the embryonic limb: stimulation of mesenchymal condensation and fibronectin gene expression by exogenenous TGF-beta and evidence for endogenous TGF-beta-like activity. Dev Biol. 1991; 145: 99-109. Ref.: https://goo.gl/DiU7mqb
- Song JJ, Aswad R, Kanaan RA, Rico MC, Owen TA, et al. Connective tissue growth factor (CTGF) acts as a downstream mediator of TGF-beta1 to induce mesenchymal cell condensation. J Cell Physiol. 2007; 210: 398-410. Ref.: https://goo.gl/GRRnTH
- Hinck AP. Structural studies of the TGF-betas and their receptors - insights into evolution of the TGF-beta superfamily. FEBS Lett. 2012; 586: 1860-1870. Ref.: https://goo.gl/3xdcFi
- ten Dijke P, Yamashita H, Ichijo H, Franzén P, Laiho M, et al. Characterization of type I receptors for transforming growth factor-beta and activin. Science. 1994; 264: 101-104. Ref.: https://goo.gl/2iEMGc
- Hecht J, Seitz V, Urban M, Wagner F, Robinson PN, et al. Detection of novel skeletogenesis target genes by comprehensive analysis of a Runx2(-/-) mouse model. Gene Expr Patterns. 2007; 7: 102-112. Ref.: https://goo.gl/hiWmYh
- Wu Q, Kim KO, Sampson ER, Chen D, Awad H, et al. Induction of an osteoarthritis-like phenotype and degradation of phosphorylated Smad3 by Smurf2 in transgenic mice. Arthritis Rheum. 2008; 58: 3132-3144. Ref.: https://goo.gl/7SH4Ns
- Habuchi H, Conrad HE, Glaser JH. Coordinate regulation of collagen and alkaline phosphatase levels in chick embryo chondrocytes. J Biol Chem. 1985; 260: 13029-13034. Ref.: https://goo.gl/NzxwKB
- Leboy PS, Vaias L, Uschmann B, Golub E, Adams SL, et al. Ascorbic acid induces alkaline phosphatase, type X collagen, and calcium deposition in cultured chick chondrocytes. J Biol Chem. 1989; 264: 17281-17286. Ref.: https://goo.gl/MKrR3F
- Farquharson C, Berry JL, Mawer EB, Seawright E, Whitehead CC. Ascorbic acid-induced chondrocyte terminal differentiation: the role of the extracellular matrix and 1,25-dihydroxyvitamin D. Eur J Cell Biol. 1998; 76: 110-118. Ref.: https://goo.gl/xHRN6D
- Li Y, Ge C, Franceschi RT. Differentiation-dependent association of phosphorylated extracellular signal-regulated kinase with the chromatin of osteoblast-related genes. J Bone Miner Res. 2010; 25: 154-163. Ref.: https://goo.gl/472SbC
- Kaiser M, Haag J, Soder S, Bau B, Aigner T. Bone morphogenetic protein and transforming growth factor beta inhibitory Smads 6 and 7 are expressed in human adult normal and osteoarthritic cartilage in vivo and are differentially regulated in vitro by interleukin-1beta. Arthritis Rheum. 2004; 50: 3535-3540. Ref.: https://goo.gl/79L8T5b
- Mansour J. Biomechanics of Cartilage. In: Oatis CA, editor. Kinesiology: the Mechanics and Pathomechanics of Human Movement. Philadelphia: Lippincott Williams and Wilkins. 2003; 66-79. Ref.: https://goo.gl/6E2U2N
- Ateshian G, Hung C. Functional properties of native articular cartilage. Functional Tissue Engineering. 2003; 46-68. Ref.: https://goo.gl/u3Vzhc
- Cui JH, Park SR, Park K, Choi BH, Min BH. Preconditioning of mesenchymal stem cells with low-intensity ultrasound for cartilage formation in vivo. Tissue Eng. 2007; 13: 351-360. Ref.: https://goo.gl/6ZejUD
- Lysdahl H, Baatrup A, Foldager CB, Bünger C. Preconditioning human mesenchymal stem cells with a low concentration of BMP2 stimulates proliferation and osteogenic differentiation in vitro. Biores Open Access. 2014; 3: 278-285. Ref.: https://goo.gl/5isdsY
- Xiao Y, Peperzak V, van Rijn L, Borst J, de Bruijn JD. Dexamethasone treatment during the expansion phase maintains stemness of bone marrow mesenchymal stem cells. J Tissue Eng Regen Med. 2010; 4: 374-386. Ref.: https://goo.gl/YDwchm
- Lee SS, Joo YS, Kim WU, Min DJ, Min JK, et al. Vascular endothelial growth factor levels in the serum and synovial fluid of patients with rheumatoid arthritis. Clin Exp Rheumatol. 2001; 19: 321-324. Ref.: https://goo.gl/BfE6ZC
- Shanmugasundaram S, Logan-Mauney S, Burgos K, Nurminskaya M. Tissue transglutaminase regulates chondrogenesis in mesenchymal stem cells on collagen type XI matrices. Amino Acids. 2012; 42: 1045-1053. Ref.: https://goo.gl/S8EfNc
- Ai M, Cui Y, Sy MS, Lee DM, Zhang LX, et al. Anti-lubricin monoclonal antibodies created using lubricin-knockout mice immunodetect lubricin in several species and in patients with healthy and diseased joints. PLoS One. 2015; 10: 0116237. Ref.: https://goo.gl/Bpy9Lo
- Han Y, Kim CY, Cheong H, Lee KY. Osterix represses adipogenesis by negatively regulating PPARgamma transcriptional activity. Sci Rep. 2016; 6: 35655. Ref.: https://goo.gl/ZCjPkk
- Yang Z, Zou Y, Guo XM, Tan HS, Denslin V, et al. Temporal activation of beta-catenin signaling in the chondrogenic process of mesenchymal stem cells affects the phenotype of the cartilage generated. Stem Cells Dev. 2012; 21: 1966-1976. Ref.: https://goo.gl/tdD53N
- Buxton AN, Bahney CS, Yoo JU, et al. Temporal exposure to chondrogenic factors modulates human mesenchymal stem cell chondrogenesis in hydrogels. Tissue Eng Part A. 2011; 17: 371-380. Ref.: https://goo.gl/u6DroQ
- Chimal-Monroy J, Rodriguez-Leon J, Montero JA, Gañan Y, Macias D, et al. Analysis of the molecular cascade responsible for mesodermal limb chondrogenesis: Sox genes and BMP signaling. Dev Biol. 2003; 257: 292-301. Ref.: https://goo.gl/jLfk2a
- Estes BT, Wu AW, Guilak F. Potent induction of chondrocytic differentiation of human adipose-derived adult stem cells by bone morphogenetic protein 6. Arthritis Rheum. 2006; 54: 1222-1232. Ref.: https://goo.gl/wrAoiR
Figures:

Figure 1
Figure 2

Figure 3

Figure 4
Figure 5
Figure 6

Figure 7

Figure 8

Figure 9

Figure 10
Similar Articles
-
Enhancing adipose stem cell chondrogenesis: A study on the roles of dexamethasone, transforming growth factor β3 and ascorbate supplements and their combinationBernard J Van Wie*,Arshan Nazempour##,Chrystal R Quisenberry##,Nehal I Abu-Lail. Enhancing adipose stem cell chondrogenesis: A study on the roles of dexamethasone, transforming growth factor β3 and ascorbate supplements and their combination. . 2017 doi: 10.29328/journal.jsctt.1001004; 1: 028-051
-
A flow perfusion bioreactor with controlled mechanical stimulation: Application in cartilage tissue engineering and beyondBernard J Van Wie*,Arshan Nazempour. A flow perfusion bioreactor with controlled mechanical stimulation: Application in cartilage tissue engineering and beyond. . 2018 doi: 10.29328/journal.jsctt.1001011; 2: 015-034
Recently Viewed
-
Extraction of DNA from face mask recovered from a kidnapping sceneBassey Nsor*,Inuwa HM. Extraction of DNA from face mask recovered from a kidnapping scene. J Forensic Sci Res. 2022: doi: 10.29328/journal.jfsr.1001029; 6: 001-005
-
Sensitivity and Intertextile variance of amylase paper for saliva detectionAlexander Lotozynski*. Sensitivity and Intertextile variance of amylase paper for saliva detection. J Forensic Sci Res. 2020: doi: 10.29328/journal.jfsr.1001017; 4: 001-003
-
The Ketogenic Diet: The Ke(y) - to Success? A Review of Weight Loss, Lipids, and Cardiovascular RiskAngela H Boal*, Christina Kanonidou. The Ketogenic Diet: The Ke(y) - to Success? A Review of Weight Loss, Lipids, and Cardiovascular Risk. J Cardiol Cardiovasc Med. 2024: doi: 10.29328/journal.jccm.1001178; 9: 052-057
-
Could apple cider vinegar be used for health improvement and weight loss?Alexander V Sirotkin*. Could apple cider vinegar be used for health improvement and weight loss?. New Insights Obes Gene Beyond. 2021: doi: 10.29328/journal.niogb.1001016; 5: 014-016
-
Maximizing the Potential of Ketogenic Dieting as a Potent, Safe, Easy-to-Apply and Cost-Effective Anti-Cancer TherapySimeon Ikechukwu Egba*,Daniel Chigbo. Maximizing the Potential of Ketogenic Dieting as a Potent, Safe, Easy-to-Apply and Cost-Effective Anti-Cancer Therapy. Arch Cancer Sci Ther. 2025: doi: 10.29328/journal.acst.1001047; 9: 001-005
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."